The prevalence of balance deficits increases with age and is associated with an increased incidence of falls seen in the elderly. Unfortunately, these falls are associated with significant morbidity and mortality (1).
Remarkably, in 2021 falls were Australia’s number one cause of injury hospitalisation and death, representing 42% of injury hospitalisations and 40% of injury deaths (4).
Additionally, the mortality risk in the 12-months post-hip fracture (common injury following a fall) is exceptionally high. Older adults (aged 65+) requiring surgery for a hip fracture are 3-4 times more likely to die within one-year, when compared with the general (younger) population (5).
For these reasons, at Restart we are big advocates of balance training especially when working with middle-aged and older patients.
What is balance?
To maintain balance, an individual’s centre of mass must stay within the changing base of support (1). Maintaining balance, when broken down into its individual components, can sound very complex – postural control depends on multiple sensory inputs:
- Somatosensory information from muscles and joints;
- Sensory information from the plantar surface (bottom) of the feet to identify surface characteristics of what you’re standing on;
- Vestibular (inner ear) information for head and trunk orientation in space;
- Gravity information from ‘gravireceptors’ in the trunk; and
- Visual input (1).
Of course, this input is sourced and processed by our bodies in nanoseconds without any conscious thought on our behalf. It isn’t until we notice that we’re bumping into more objects around the house, listing to one side when walking, or worst case scenario, have a trip or fall, that balance becomes a concern.
There’s a discernable lag in how well we’re adapting and responding to the world around us.
Elderly adults show age-related decline in sensory systems and reduced ability to adapt to changes in their environment to maintain balance. Elderly adults are particularly dependent on vision to maintain postural stability (1). This points to the importance of a well-rounded balance program to target each of the five balance systems listed above.
Is my balance deteriorating?
Try this exercise to determine whether your balance may be deteriorating.
Simply stand with feet together on a firm surface, and close your eyes for 60 seconds. Have someone observe you to maintain safety.
Do you sway from side to side, front to back?
Is it more challenging than you expected?
Older subjects were found to have a ‘sway velocity’ four times that of younger subjects with eyes closed (1). It is this sway velocity and inability to maintain a static position with eyes closed that can be one of numerous predictors for increased falls risk.
Connection between strength and balance
In addition to sensory input, decreased muscle strength also impairs balance in the elderly. For each Nm/kg (Newton metre per kilogram – measure of torque) increase in leg muscle strength, the adjusted odds of losing balance decrease by 20% (1). Simply put, stronger legs = decreased falls risk.
This points to the importance of regularly engaging in resistance training throughout all stages of life, and adhering to the physical activity guidelines of achieving at least two bouts of strength training per week.
Is my leg strength deteriorating?
Find a chair at home with a straight back, no arms rest, and seat height 43cm off the ground.
Have someone stand next to you and time how many sit-to-stands you can perform in 30 seconds. To ensure proper technique, cross your arms, keep your feet flat, sit back to the back rest, and achieve a full standing position.
How many repetitions did you complete in 30 seconds?
The below graph illustrates a below average score for ages beyond 60 for men and women.
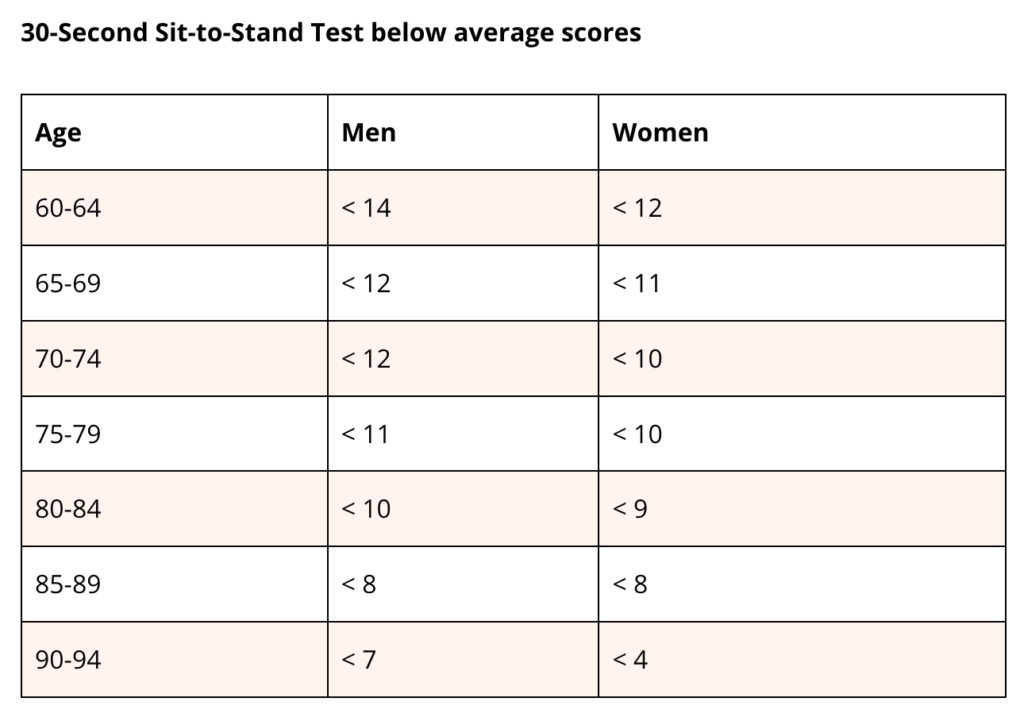
If you completed less than the above score for your age and gender, your risk of falls is greater than it could be.
Simply completing a greater number of sit-to-stands every days should see your leg strength improve and associated falls risk reduce. Try performing 10 reps each morning, lunchtime and evening as a daily habit. For a more comprehensive approach, consult with an Exercise Physiologist to develop a suitable lower-body strengthening program to know you’re doing all you can to build strong legs and better balance.
Has your gait (walking) changed recently?
Some patterns of gait disturbance arise particularly in old age, which can be traced back to sensory deficits. Stability, or lack thereof, is an important marker of gait in the elderly (1).
‘Worse’ gait is defined as:
- Increased gait variability (step-to-step variations);
- Shorter stride/step length;
- Slower walking speed;
- Increased % of the gait cycle spent in double-leg support and stance;
- Decreased stride width with increased stride width variability, and
- Less accurate tandem walking.
If you’ve noticed a deterioration in your walking recently, try the following…
Set up a camera in your hallway or backyard and walk back and forwards towards it a handful of times.
Do you notice an inability to walk in a straight line?
Are some steps narrow, and some wider?
Do you hear your feet scuffing against the ground?
In assessing falls risk, studies show that adults at high risk of falling demonstrate a significantly slower gait speed as a result of shorter step length (3).
If you’ve noticed that you can’t keep up with your partner at the shops, or a general tendency that you’re slowing down, it could be time to ask for help.
The strongest indicator for falls risk is of course suffering frequent falls. Have you had a fall recently, and recognise a loss of confidence in tackling day to day activities?
Has your walking slowed down? Did you score below your age norm for the 30s sit-to-stand test? Was standing with feet together and eyes closed more difficult than you expected?
Next step
Having read the above, you now know the indicators for deteriorating balance – the good news is that with frequent balance training, balance can be improved at any age. We’ve helped patients of all ages, including patients in their 80s and 90s improve their balance via guided, safe and appropriate balance and strength training.
To gain the best support in this area, call Restart on 1300 899 757 or book online today.
References
- Osaba, M.Y., Rao, A.K., Agrawal, S.K. Balance and gait in the elderly: A contemporary review. Laryngoscope Investig Otolaryngol Feb; 4(1): 143–153 (2019). doi: 1002/lio2.252
- Injury Matters: Prevention to Recovery, retrieved 19th June 2023 from https://www.injurymatters.org.au/programs/stay-on-your-feet/information-for-health-and-community-workers/falls-screening-and-assessment-tools/sit-to-stand-tests
- Figueiro MG, Plitnick B, Rea MS, Gras LZ, Rea MS. Lighting and perceptual cues: effects on gait measures of older adults at high and low risk for falls. BMC Geriatr2011;11:49.
- Australian Institute of Health and Welfare, retrieved 19th June 2023 from https://www.aihw.gov.au/reports/injury/falls
- Morri, M., Ambrosi, E., Chiari, P. et al.One-year mortality after hip fracture surgery and prognostic factors: a prospective cohort study. Sci Rep 9, 18718 (2019). https://doi.org/10.1038/s41598-019-55196-6
0 Comments